What You Need to Know
- The witness for the ERISA Industry Committee said employers added everything from yoga classes to crisis hotlines.
- He said temporary flexibility for HSA users ends Jan. 1.
- Other witnesses talked about the impact of narrow behavioral health provider networks.
Large employers are asking Congress to make it easier for health savings account (HSA) holders to get some mental health care for no or low cost, before they meet their deductibles.
During a live-streamed House Education and Labor health subcommittee hearing on behavioral and mental health care access, James Gelfand, a senior vice president for health policy at The ERISA Industry Committee, talked about the effects of current HSA program rules on mental health care.
Rep. Mark DeSaulnier, D-Calif., the health subcommittee chairman, said in opening remarks to last week’s meeting that about 41% of U.S. adults surveyed now report symptoms of depression or anxiety, up from 11% about a year ago, before the COVID-19 pandemic began.
“Individuals seeking affordable mental health services are facing significant barriers,” DeSaulnier said.
Provider Networks
One obstacle is a shortage of providers. A second is lack of true health insurance parity between coverage for mental health services and other types of health services, in spite of the existence of the Mental Health Parity and Addiction Equity Act of 2008 and other federal parity laws and regulations, DeSaulnier said.
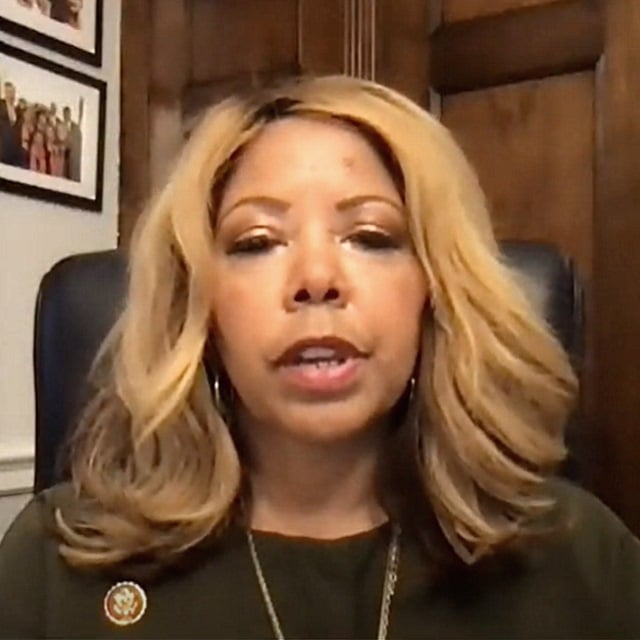
Rep. Lucy McBath, D-Ga., said the pandemic has laid bare many of the inequities of the U.S. health care system.
“I have seen a host of disparities develop and worsen with the onset of this pandemic, even within my own constituency,” McBath said.
McBath and other lawmakers and witnesses also discussed the role of health insurer reimbursement rates and narrow networks in limiting access to mental health and behavioral care.
Health Account Rules
Gelfand, who spoke for a group that represents employers with self-insured health plans, said that the plans already are trying to provide good mental and behavioral benefits, and that new mandates and penalties won’t improve the situation.
He said plans have done everything from adding online meditation and yoga classes to setting up crisis hotlines to help get employees through the pandemic.
Congress could help by making it easier for a provider in one state to counsel a patient in another state through a telehealth system, he said.
That could help plans deal with the problem that mental health professionals often prefer to live in big cities, rather than in small towns and rural areas, Gelfand said.
He also called for Congress to update the rules governing HSAs. The current rules require HSA users to combine HSAs with high-deductible health plans. The minimum HSA deductible for 2021 is $1,400 for an individual and $2,800 for a family.
The high-deductible plans must cover annual checkups and some screening tests with no out-of-pocket costs for the patients.
Gelfand said Congress should also allow for “first-dollar coverage” for some mental health and behavioral health care.
“Last year, Congress temporarily allowed first-dollar coverage of telehealth,” Gelfand said. “We should make it permanent, and add coverage of worksite health clinics, too. If Congress doesn’t act, starting on Jan. 1, tens of millions of patients will have to pay their entire deductible before employers can subsidize these benefits.”
(Photo: Shutterstock)







 April 19, 2021 at 02:00 PM
April 19, 2021 at 02:00 PM













 Slideshow
Slideshow





