Mental Health Parity in the US: Have We Made Any Real Progress?
A breakdown of how we are living up to the ideals and standards proposed by the 2008 Mental Health Parity and Addiction Equity Act, including the pandemic's impact on parity.
Mental Health Parity Rankings
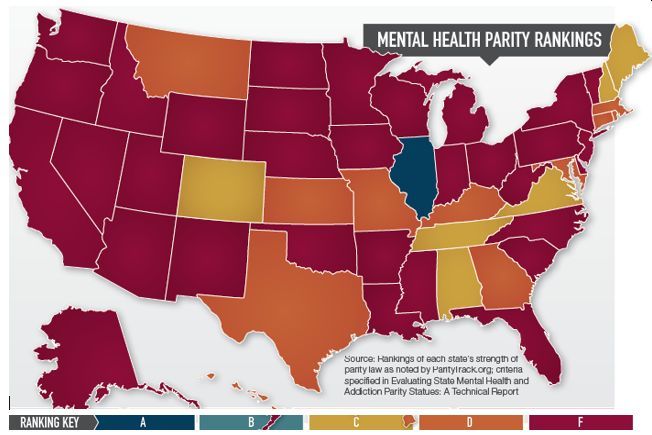
Figure. Types of violations found in DOL enforcement actions, FY 2010–2015
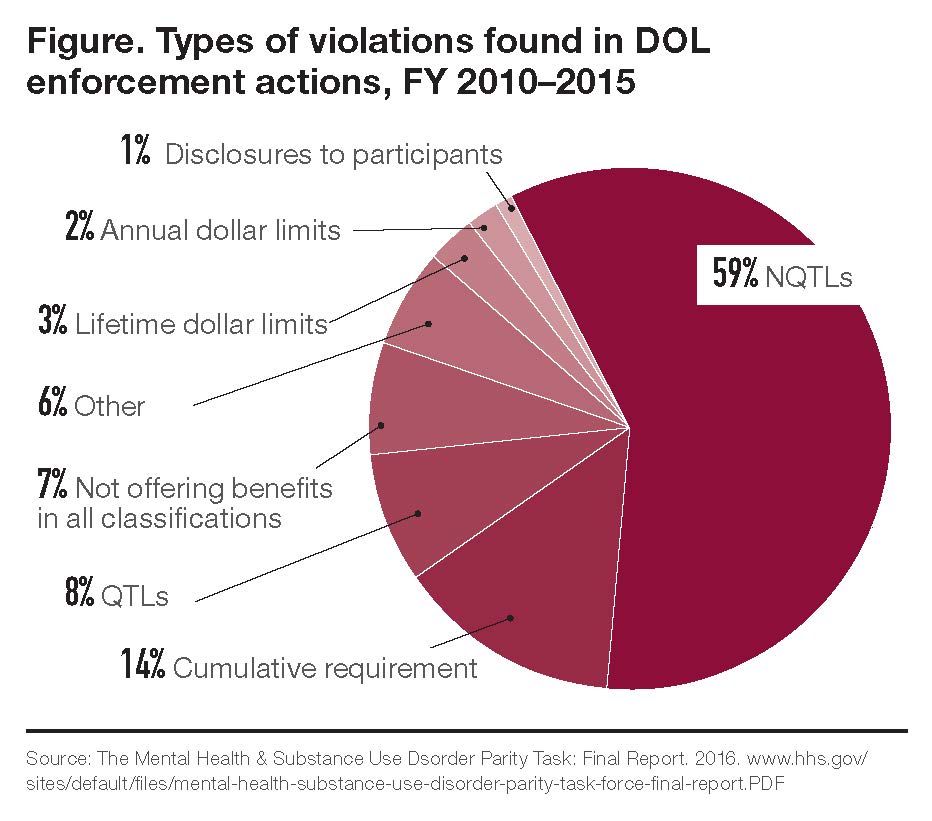
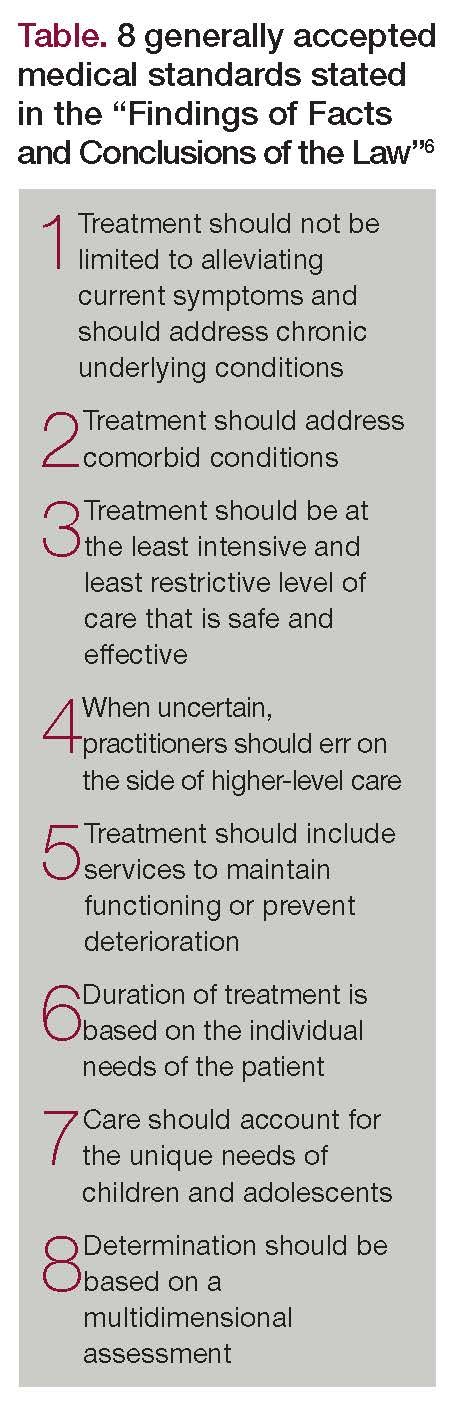
Table. 8 generally accepted medical standards stated in the “Findings of Facts and Conclusions of the Law”[6]
Are we living up to the ideals and standards proposed by the 2008 Mental Health Parity and Addiction Equity Act (MHPAEA)? According to some recent reports and measures, the answer is no. Mental health parity is a straightforward concept: insurance coverage for mental health conditions, including substance abuse disorder (SUD) treatment, should be equal to coverage for any other medical conditions. While the MHPAEA codified the idea in federal and state law, its implementation has proved difficult.
Reviewing the report cards
In late 2019, Milliman1 released a report card of sorts looking at the status of mental health parity based on insurance information. In the 140-page research report, Addiction and Mental Health vs. Physical Health: Widening Disparities in Network Use and Provider Reimbursement, the updated information from 2017 showed continued and increased disparities between behavioral health care and physical health care coverage, indicating possible evidence of noncompliant insurance practices.
The report, which examined claims data for more than 37 million employees and dependents from all 50 states, included the following findings:
1 Disparity in the use of out-of-network inpatient services. In 2013, behavioral health care providers were 2.8 times more likely than their medical or surgical counterparts to see a patient who was going out of network; in 2017, they were 5.2 times more likely (an 85% increase).
2 Disparity for out-of-network behavioral health office visits relative to medical or surgical primary care office visits increased from 5.0 times (500%) more likely in 2013 to 5.4 times (540%) more likely in 2017 (an 8% increase).
3 In 2017, reimbursement rates for primary care office visits were more than 50% higher than those for behavioral health office visits in 11 states. Further, the reimbursement rates for primary care office visits were between 30% and 49% higher than those for behavioral health office visits in an additional 13 states.
4 Disparity between how often SUD inpatient facilities are utilized out of network relative to medical or surgical inpatient facilities increased from 4.7 times more likely in 2013 to 10.1 times more likely in 2017.
“The Milliman findings emphasize what our members have been telling us for years: unfair managed care practices too often create barriers for patients to access the care they need,” noted Mark Covall, executive vice chairman of the National Association for Behavioral Healthcare. “This is a major reason why earlier this year we launched Access to Care, an initiative to inform policymakers, the media, patient advocates, and the general public about two major challenges—unjust managed care practices and countless regulations—that prevent behavioral health care providers from providing a full range of services to patients.”
Although it is the most recent to examine the issue, the Milliman report is not alone in finding evidence of disparity, despite the MHPAEA’s good intentions. In 2013, the Health Care Cost Institute (HCCI) shared results from their analysis of mental health, substance use, and medical or surgical inpatient per capita spending. The information included utilization, prices, and out-of-pocket payments for those under the age of 65, covered by employer-sponsored health insurance.2 The institute found that spending on mental health and substance use admissions increased faster than other subcategories between 2013 to 2017, but still accounted for a relatively small share of total spending in 2017. HCCI further noted that year-over-year increases in the average price of mental health and substance use admissions tracked the other subcategories of inpatient admissions between 2013 and 2015. From 2015 to 2017, average prices rose more sharply, resulting in a cumulative increase of 23%, the largest in percentage terms of any subcategory. HCCI, which was funded by insurance companies, ultimately concluded the results were unclear.
In a more general study, in 2018, the Cohen Veterans Network found that “American mental health services are insufficient, and despite high demand, the root of the problem is lack of access—or the ability to find care.” Results from their study indicate that 53 million Americans (21%) wanted to see a mental health care professional at some point but were unable to do so due to “reasons outside of their control.”3 Furthermore, 55% of Americans believe there needs to be a shift in society to make mental health care a priority. Those in rural area and those with low incomes (less than $49,999 annually) were less likely to report proper access to care (39% and 42%, respectively).
The report noted that cost or poor insurance coverage was the top barrier to seeking effective mental health services for Americans. Alarmingly, 1 in 4 Americans had to choose between mental health care treatment and paying for daily necessities, and 1 in 5 had to choose between treatment for a physical condition or a mental health condition because of costs.
Parity law in action—or is it inaction?
Why hasn’t the legislation done enough to halt disparity? Angela Kimball, national director of advocacy and public policy for the National Alliance on Mental Illness (NAMI), says it is largely a problem of enforcement. “There is a lack of oversight and efforts to make sure that health plans are compliant with not only the letter of the law, but the spirit of law,” said Kimball. This is one reason why NAMI undersigned a letter to congress on March 13, 2020, concerning the lack of parity oversight.
Kimball explained that the American health care system includes a large number of competing for-profit insurers, creating more variation in parity enforcement. Countries with a single-payer health care system often see the value in providing mental health care, and consequently, have fewer parity problems than the United States.
“Say you work for a big company like Intel or Google—your self-insured health plan is actually under the jurisdiction of the federal department of labor,” explained Kimball. “But many other health insurance plans are under the authority of their state insurance division. So, we have a lot of different kinds of health insurance that are subject to very different rules and sometimes different government agencies.” As there is no single way to enforce parity, it is easier for noncompliant insurers to avoid getting caught.
Similarly, parity discrepancies from state to state derive from different levels of insurer competition or the independent, consumer-friendly nature of each state’s insurance division. Although some states are more aggressive in ensuring parity, Kimball would not say that any state is doing it perfectly. “For example, Maryland’s attorney general just came out with 6 or 7 settlement agreements against a number of different insurers operating in that state for violations of parity,” said Kimball. “You have other states that don’t enforce [parity] at all.”
Indeed, states vary in their approach to parity legislation. In Connecticut, a mental health parity bill was recently signed into law that requires insurance providers to submit annual reports detailing their mental health or SUD coverage.4 The bill takes effect next year and requires providers to cover drugs prescribed for substance abuse treatment.
In a recent interview, Kentucky State Representative Lisa Willner advocated for reinvestment in the state’s mental health parity laws.5
We can keep doing what we’re doing and continue to see those systems lose support, lose funding, lose personnel, lose expertise, lose their attractiveness as training centers for new mental health providers. . . or, we could raise revenue in the state, we could invest in these social safety net services.
Among many solutions, Willner proposed building mental health centers and adding providers, and urged citizens to make their message clear to state legislators.
Mental health parity litigation
Violations of parity law revolving around MHPAEA guidelines include comparing the treatment limitations of a plan’s mental health or SUD benefits to its medical or surgical benefits. In terms of quantitative treatment limits, such as the number of visits allowed to a mental health professional, insurers are generally compliant with MHPAEA guidelines (Figure).
Most parity lawsuits deal with nonquantitative treatment limits such as preauthorization requirements for mental health or SUD services, residential treatment limitations, and unequal fail-first protocols.6 According to a report on the Health Affairs blog, fail-first protocols, which is when plans require a patient to try a cheaper alternative to a medication first, is one of the most common types of coverage restrictions in the United States.7
Health plan benefits are evaluated for parity within the following categories: inpatient in-network, inpatient out-of-network, outpatient in-network, outpatient out-of-network, emergency services, and drugs. Legally, plans compliant with parity law ensure that no standard is being applied more stringently for mental health or SUD benefits than for medical or surgical benefits.
One of the most significant cases of mental health parity litigation was Wit v United Behavioral Health (UBH) in North California in 2019. The allegation was that UBH’s coverage of mental health or SUD treatment was more restrictive than “generally accepted medical standards.”8 A federal judge ruled that UBH had created discriminatory policies for patients with mental health and substance abuse disorders in order to save money. The court found all of UBH’s guidelines to be more restrictive than generally accepted medical standards. The guidelines described in the case’s “Findings of Facts and Conclusions of the Law” report were based on industry standards, the Centers for Medicare & Medicaid Services’ manual, and expert opinion (Table).6
In a second parity lawsuit, Smith v UBH, the company was accused of underpaying out-of-network therapists. The allegation claimed that UBH’s provision to reduce therapists’ rate by 25% to 35% was discriminatory under the MHPAEA.6 The court ruled that UBH did indeed violate parity law.
Similar financial discriminatory practices may worsen ongoing shortages in the mental health workforce. A report from the Health Resources and Services Administration projects shortages in the number of psychiatrists and addiction counselors by 2030 if today’s level of behavioral health care utilization remains the same.9
In February this year, 5 large insurers and 2 behavioral health care companies settled a parity claim with the state of Massachusetts, agreeing to pay $1 million.10 The defendants were accused of: having inaccurate directories, under-reimbursing mental health services, and requiring prior authorization for routine behavioral health visits. In the same month, the Massachusetts Senate unanimously passed a bill to help support the mechanisms underlying parity.11 Such mechanisms include expanding the mental health practitioner workforce and seeking a rate floor to ensure mental health clinicians and primary care providers are paid the same for similar services.
The pandemic’s impact on parity
Headlines during the COVID-19 pandemic have highlighted the need for mental health and mental health parity. According to a recent Kaiser Family Foundation (KFF) report, a KFF poll conducted March 25 through March 30 showed that 45% of Americans said COVID-19 had negatively affected their mental health.12 Likewise, a March 29 McKinsey & Company survey investigated signs of distress related to COVID-19: 1 out of 4 people reported binge drinking, 1 out of 5 reported taking prescription drugs for nonmedical use, and 1 out of 7 reported using illicit drugs.13
According to Kimball, about 1 in 5 people in the United States were already suffering from a mental health condition. So, when Americans suddenly lost their jobs, experienced financial pressures, and became isolated, their symptoms were exacerbated.
“People are recognizing that this is an issue because they’re feeling it in a very immediate way, and I think policymakers are recognizing this as well,” said Kimball. “In their own staff, their families, and themselves, they are seeing this is real.” Kimball hopes this sparks a renewed interest in making sure our health coverage system covers mental health fairly.
Fortunately, there is one area of parity for mental health in this country. The Americans With Disabilities Act (ADA) prohibits discrimination against employees with physical or mental impairment that “substantially limits one or more major life activity.” This includes diagnosed mental illnesses. As such, sick days can be used to address mental health distress, including new issues as well as worsening preexisting conditions. Undiagnosed mental health conditions work in the same way as an undiagnosed cold or flu—they are grounds for a sick day, and you do not have to specify what symptoms you are experiencing.
Mental health sick days are better prioritized now than ever before. So far, this legislation has focused on schools granting mental health absences. Kimball explained:
Young people are the main movers and shakers of legislation that’s happening around the country to provide mental health days... I think it really signals that tomorrow’s generation is not going to put up with the disparate treatment of mental health and substance abuse conditions that other generations have been content with and tolerated. We’re still seeing discrimination and marginalization of people with mental health conditions and in mental health care. . . . but thankfully, I think public perceptions are changing and they’re changing most rapidly amongst the young. And that gives me hope.
Ali Shana is a freelance writer. He is currently studying clinical mental health counseling at the University of Milwaukee-Wisconsin. He reports on rehabilitation, drug policy reform, and health care issues.
References
1. Davenport S, Gray TJ, Melek SP. Addiction and mental health vs. physical health: widening disparities in network use and provider reimbursement. Milliman Research Report. 2019.
2. 2017 Health care cost and utilization report. Health Care Cost Institute. February 2019. www.healthcostinstitute.org/images/easyblog_articles/276/HCCI-2017-Health-Care-Cost-and-Utilization-Report-02.12.19.pdf. Accessed May 14, 2020.
3. Cohen Veterans Network. America’s Mental Health 2018. National Council for Behavioral Health. 2018.
4. Carlesso J. Mental health parity bill signed into law. CT Mirror. July 8, 2019. Accessed https://ctmirror.org/2019/07/08/mental-health-parity-bill-signed-into-law. May 14, 2020.
5. Jackson C. State Rep. Lisa Willner: Kentucky needs to reinvest in mental health safety net. WKU Public Radio. March 13, 2020.
6. Mannat, Phelps & Phillips, LLP. Understanding mental health parity: insurer compliance and recent litigation. JD Supra. November 22, 2019.
7. Chambers JD, Panzer AD, Neumann PJ. Variation in the use of step therapy protocols across US health plans. Health Affairs blog. September 14, 2018. www.healthaffairs.org/do/10.1377/hblog20180912.
391231/full/. Accessed May 14, 2020.
8. Abelson R. Mental Health Treatment Denied to Customers by Giant Insurers’ Policies, Judge Rules. New York Times. March 5, 2019.
9. Health Resources and Services Administration. Behavioral Health Workforce Projections, 2017-2030. National Center for Health Workforce Analysis. 2020.
10. Bartlett J. Insurers sign $1M settlement with Healy over mental health parity. Boston Business Journal. February 27, 2020.
11. Lisinski C. Mass. Senate Passes Bill to Boost Mental Health Care Access. WGHB. February 14, 2020.
12. Kirzinger A, Kearney A, Hamel L, Brodie M. KFF Health Tracking Poll—Early April 2020: The Impact of Coronavirus on Life in America. Kaiser Family Foundation. 2020. www.kff.org/coronavirus-covid-19/report/kff-health-tracking-poll-early-april-2020/. Accessed May 15, 2020.
13. Coe EH, Enomoto K. Returning to resilience: the impact of COVID-19 on mental health and substance use. McKinsey & Company. 2020. www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/helping-us-healthcare-stakeholders-understand-the-human-side-of-the-covid-19-crisis. Accessed May 15, 2020. ❒